This scientific breakthrough could revolutionize cancer treatment 🎯
Published by Cédric,
Article author: Cédric DEPOND
Source: Nature Biotechnology
Other Languages: FR, DE, ES, PT
Article author: Cédric DEPOND
Source: Nature Biotechnology
Other Languages: FR, DE, ES, PT
Follow us on Google News (click on ☆)
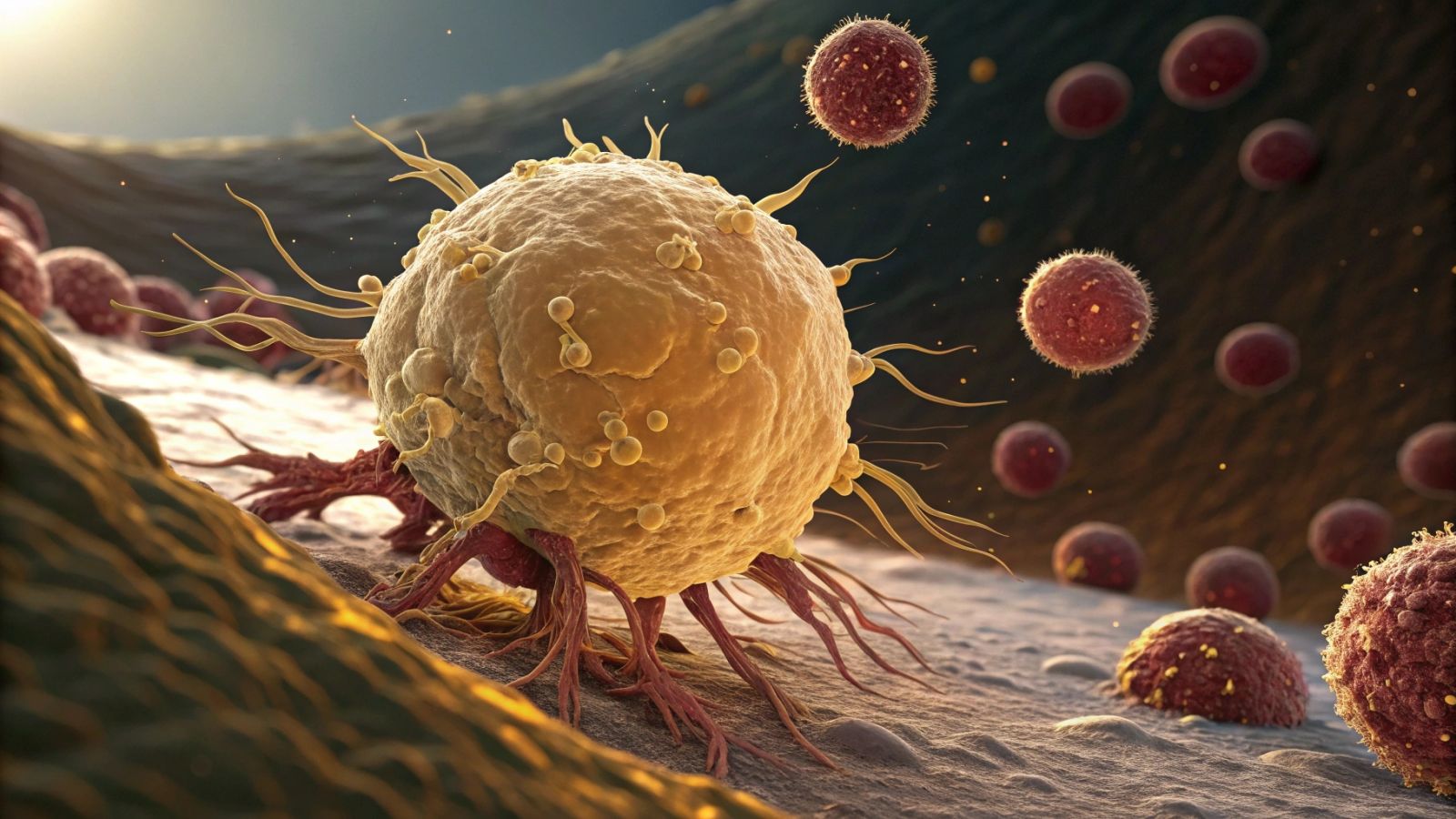
Their study, published in Nature Biotechnology, reveals that fat cells, generally perceived as simple energy reservoirs, can be genetically modified to starve cancer cells. Through advanced cellular engineering, these reprogrammed cells have demonstrated their ability to slow down or even halt the progression of several types of tumors in laboratory settings.
Turning fat cells into therapeutic allies
Fat cells are divided into three categories: white cells, which store energy; brown cells, which burn calories to produce heat; and beige cells, which combine the properties of the first two. Researchers have exploited this last category by using the CRISPR tool to activate a key gene, UCP1, which grants them enhanced metabolic capacity.
Once modified, these beige fat cells behave differently: they consume more energy and absorb the nutrients necessary for cancer cells to grow. This metabolic competition weakens tumors, which can no longer develop normally. This approach could thus offer an alternative to conventional treatments by directly depriving malignant cells of the resources they need.
A simple and adaptable protocol
One of the most promising aspects of this discovery lies in the simplicity of the process. Fat cells can be easily extracted from a patient through liposuction, modified in the laboratory, and then reinjected near the tumors. This technique, already mastered in the field of cosmetic surgery, makes the approach potentially more accessible than other complex cellular therapies.
Moreover, this method relies on cells derived from the patient's own body, which significantly reduces the risks of immune rejection. This natural compatibility could accelerate the clinical adoption of this strategy, allowing for personalized treatments based on the type and location of the cancer.
Effectiveness confirmed in the laboratory
Tests conducted have demonstrated a significant impact on five types of cancers, including breast, colon, prostate, and pancreatic cancers. In the laboratory, the modified fat cells slowed tumor proliferation by massively absorbing nutrients, thereby reducing the nourishment of cancer cells. In murine models, tumors treated with this technique showed a notable slowdown in their progression.
Surprisingly, the anticancer effect was observed even when the transformed fat cells were implanted at a distance from the tumors. This phenomenon suggests a still poorly understood mechanism of action, but one that could broaden the application prospects of this technology, particularly for hard-to-reach cancers.
Towards a new therapeutic era?
Despite these encouraging results, this approach is still in the experimental stage. It remains necessary to evaluate its long-term effects, its safety in humans, and its effectiveness on a wider variety of cancers. Clinical trials will need to be conducted to verify whether these reprogrammed cells can truly constitute a viable alternative to existing treatments.
If these researches succeed, they could pave the way for a new generation of anticancer therapies based on cellular reprogramming. Rather than directly attacking tumor cells, the idea would be to deprive them of the resources essential for their survival, a subtle approach that could revolutionize the fight against cancer.
To go further: How can fat cells starve tumors?
Cancer cells have a high energy demand to multiply rapidly. They capture large amounts of glucose and fatty acids present in their environment. By genetically modifying fat cells, researchers have given them an increased capacity to absorb these nutrients, thereby reducing the supply to tumors.
Experiments have shown that these transformed fat cells capture up to 50% more glucose than normal cells. This excessive absorption creates a metabolic competition: cancer cells are deprived of fuel, which slows their growth and can even cause their death due to lack of energy.
Another key mechanism relies on the activation of the UCP1 gene. This gene, usually active in brown fat cells, triggers intense energy consumption. By stimulating it in the modified fat cells, they burn more calories, further reducing the availability of essential nutrients for tumor cells.