Follow us on Google News (click on ☆)
Scientists from the Institut Pasteur, Inserm, AP-HP, and Université Paris Cité have developed a new tool capable of selecting, simply and efficiently, the best possible cocktail of bacteriophages for a given patient. To achieve this, they created and trained an artificial intelligence model that can tailor-select bacteriophages based solely on the genome of targeted bacteria.
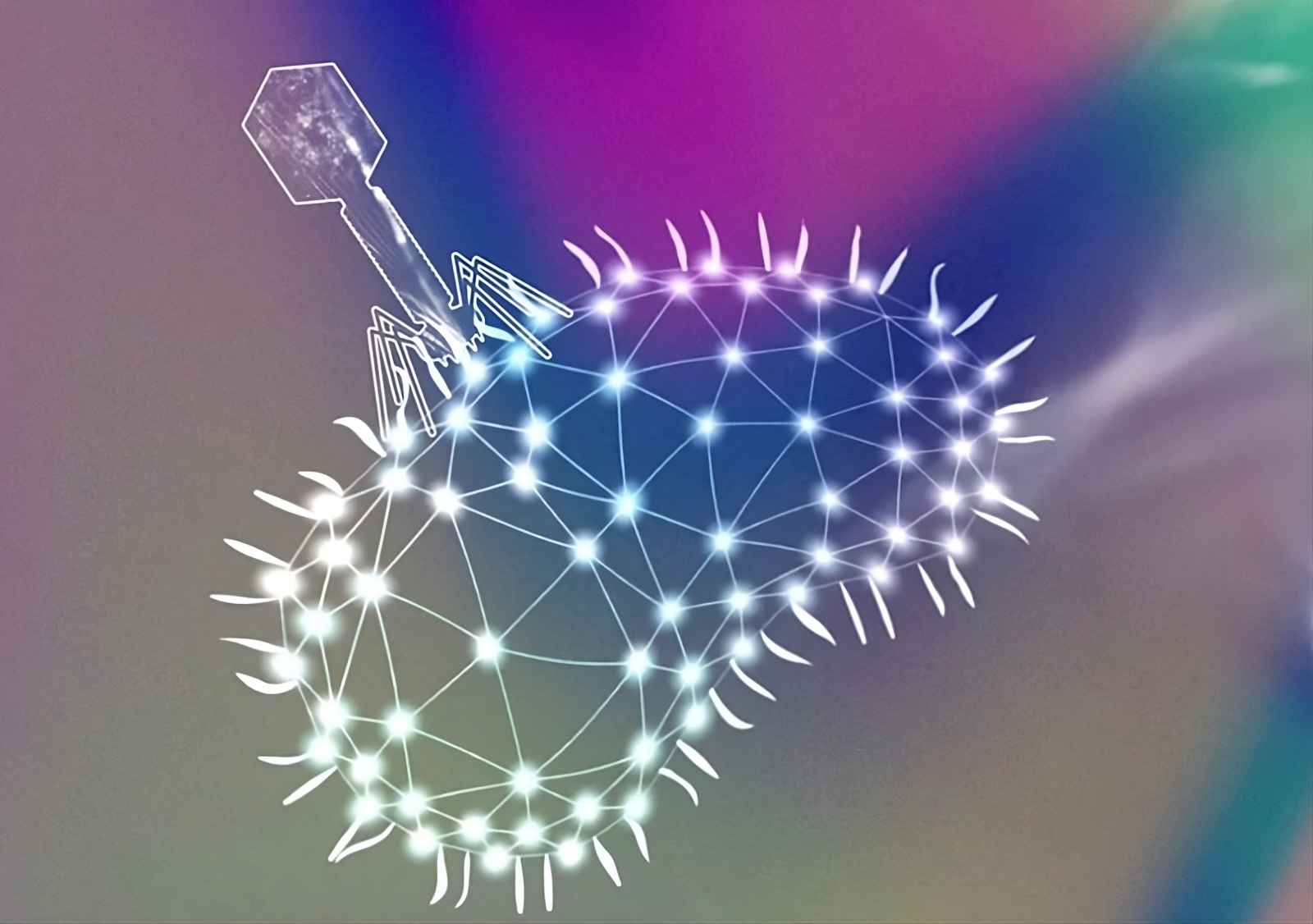
Illustration of a phage attached to a bacterium.
© Adrien Bernheim
The results of this research were published on October 31, 2024, in the journal Nature Microbiology, paving the way for personalized phage therapies to combat antibiotic-resistant bacterial infections.
Some bacteria, such as Escherichia coli, are becoming increasingly resistant to conventional antibiotics and have become what are called "superbugs." To overcome these resistances, which pose a significant public health challenge, research teams are exploring phage therapy. The principle: using viruses, known as phages or bacteriophages, which only infect bacteria, to specifically target and eliminate bacteria that are pathogenic to humans.
"Phage therapy was invented by the Pasteur researcher Félix d'Hérelle in the 1920s and was later abandoned in favor of antibiotics in the late 1930s, which were much simpler and cheaper to produce and use. Today, only a few countries in Eastern Europe, like Georgia, still utilize phage therapy, while in Western countries, 'broad-spectrum' phages are sporadically used on compassionate grounds to treat chronic, multi-resistant antibiotic infections when no authorized drug is effective anymore," explains Baptiste Gaborieau, co-lead author of the paper, intensive care physician at Louis Mourier Hospital (AP-HP), and researcher in the IAME lab (Université Paris Cité-Inserm). "For about two decades now, driven by the WHO's promotion and more recently by clinical trials, particularly in Europe, phage therapy has regained interest."
One major challenge is determining which bacteriophage will be effective against a given infection, as each phage can only infect specific bacterial strains. Phages are naturally present in soil or water and circulate until they find the right target.
Thus, scientists from the Institut Pasteur, Inserm, AP-HP, and Université Paris Cité decided to take a closer look at bacteria-phage interactions to determine if it was possible to predict a bacteriophage's effectiveness on a given bacterial strain. The first step involved creating a high-quality database, comprising 403 strains of Escherichia coli bacteria on one side and 96 bacteriophages on the other. This endeavor required more than two years of effort.
"We exposed the phages to cultured bacteria and observed which bacteria were killed. We studied 350,000 interactions and succeeded in identifying, at the genome level of the bacteria, the characteristics likely to predict the phages' effectiveness," summarizes Aude Bernheim, lead author of the study and head of the Microbes Molecular Diversity laboratory at the Institut Pasteur.
"Contrary to what was initially thought, it is the receptors on the bacterial surface—not their defense mechanisms—that primarily determine the ability of bacteriophages to infect bacteria and predict their effectiveness," adds Florian Tesson, co-lead author of the paper and a doctoral student in the Microbes Molecular Diversity laboratory at the Institut Pasteur and IAME laboratory at Université Paris Cité-Inserm.
Thanks to this precise and extensive analysis of interaction mechanisms between bacteria and phages, the team's bioinformaticians were able to design an optimized and efficient artificial intelligence program. This program relies on analyzing bacterial genomes, particularly the regions involved in coding for the bacteria's membrane receptors, which serve as the entry points for phages.
"We are not dealing with a ' black box ' here, and that's what makes our AI model so robust. We know exactly how it works, which helps us improve its performance," notes Hugo Vaysset, co-lead author of the paper and doctoral student in the Microbes Molecular Diversity laboratory at the Institut Pasteur.
After more than two years of design and training, the AI was able to correctly predict the effectiveness of bacteriophages against the E. coli bacteria in the database in 85% of cases, simply by analyzing the bacteria's DNA.
"This result exceeded our expectations," admits Aude Bernheim.
To push further, researchers tested their model on a new collection of E. coli strains responsible for pneumonia and selected a customized "cocktail" of three bacteriophages for each. In 90% of cases, the AI-selected bacteriophages successfully completed their mission, destroying the present bacteria.
This method, which can be easily implemented in hospital biology laboratories, paves the way for the rapid and personalized selection of phage therapy treatments in the coming years when addressing Escherichia coli infections highly resistant to antibiotics.
"We still need to test how the phages behave in different environments, but the proof of concept is there. We hope to extend this approach to other pathogenic bacteria since our AI was designed to adapt easily to other cases, ultimately offering personalized phage therapy treatments in the future," concludes Aude Bernheim.