Researchers revive pigs' brains 1 hour after death thanks... to their liver 🐖
Published by Cédric,
Article author: Cédric DEPOND
Source: EMBO Molecular Medicine
Other Languages: FR, DE, ES, PT
Article author: Cédric DEPOND
Source: EMBO Molecular Medicine
Other Languages: FR, DE, ES, PT
Follow us on Google News (click on ☆)
EMBO Molecular Medicine reveals a major breakthrough: Chinese scientists have managed to revive pigs' brains one hour after cardiac arrest. This feat relies on an innovative liver-based intervention.

Illustrative image Pixabay
The experiment, conducted at Sun Yat-sen University, highlights the liver's impact on brain health post-resuscitation. By incorporating this organ into the normothermic perfusion system, the researchers observed a reduction in brain damage. When the brain is deprived of oxygen following a cardiac arrest, lesions develop rapidly. In France, only 5% of cardiac arrest victims survive without neurological damage, according to the Ministry of Health.
To test their hypothesis, the scientists isolated pigs' brains and simulated a cardiac arrest. They then connected the brains to a normothermic perfusion system (to mimic blood and oxygen circulation). Some brains were also connected to a functional liver in addition to the perfusion system. Researchers noted a clear difference: the brains connected to the liver showed better resistance to damage and maintained stable electrical activity compared to those connected solely to the perfusion system.
The liver, through its metabolic functions, produces protective molecules such as ketone bodies. These substances could serve as an energy alternative in case of glucose deficiency. The results show that the liver reduces inflammation and limits brain swelling. Neurons in the cortex and hippocampus, often the first to be affected, were substantially less damaged.
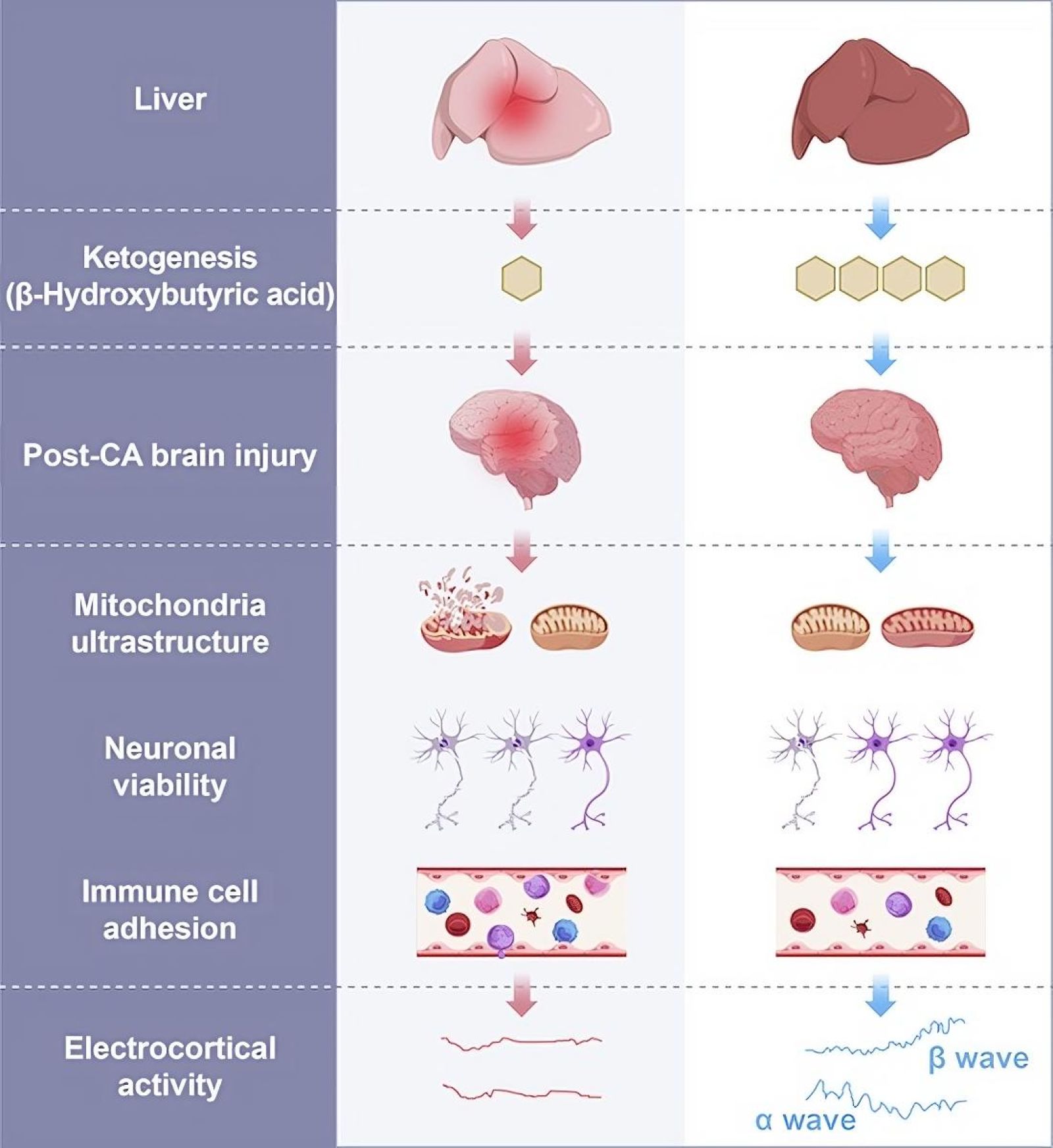
The liver's role in brain injuries after cardiac arrest was studied in a porcine model of global cerebral ischemia (lack of blood flow).
- The infarct area in the frontal lobe and the adhesion of immune cells in the temporal lobe increased in ischemic brains with concurrent liver ischemia.
- Ex vivo, the presence of a functional liver improved neuronal viability, cytoarchitecture, and electrocortical activity after brain damage caused by cardiac arrest.
- Transcriptomic and metabolomic analyses suggest that the liver protects against brain injury following cardiac arrest by increasing ketone body production.
Although this technique is not yet applicable to humans, it opens up possibilities for extending the resuscitation window and thus increasing chances of survival.
How does the liver protect the brain after cardiac arrest?
The liver is a vital organ, central to the body's metabolism and detoxification. During cardiac arrest, it plays a key role by producing molecules, such as ketone bodies, which replace glucose as the brain's energy source.
By reducing inflammation and purifying the blood, the liver helps to limit brain damage after cardiac arrest. Its action slows down neuronal degradation processes, allowing for more effective brain resuscitation by preserving its structure and function.
How important is the resuscitation window after a cardiac arrest?
The resuscitation window refers to the critical period during which a patient's vital functions can be most successfully restored after a cardiac arrest. Typically, this window lasts only a few minutes, as after that time the brain begins to suffer irreversible damage due to lack of oxygen.
If blood flow is not quickly restored, nerve cells begin to die, leading to severe or even fatal brain damage. Recent advancements, such as those achieved by Chinese researchers, indicate that by extending this window through specific interventions, it may be possible to improve survival rates and neurological outcomes in cardiac arrest victims.