🩺 Effective diabetes medications to fight cancer
Follow us on Google News (click on ☆)
A link between type 2 diabetes and a higher risk for certain cancers, such as liver or colon cancer, is already recognized. However, the usual explanations, such as excess sugar in the blood or overweight, do not seem sufficient. This observation has therefore directed research towards an original lead: could the molecules prescribed against diabetes play a direct role in tumor biology?
An analysis published on December 10, 2025, in the journal Clinical Precision Medicine examines this hypothesis. This work reviews several classes of medications, including metformin, SGLT2 inhibitors, and GLP-1 receptor agonists. It reveals that these treatments are likely to modify fundamental processes for cancers. Their actions could thus affect the speed of cell multiplication, the regulation of inflammation, or even the immune system's response.
Take the example of metformin, a very widespread medication. It seems to interact with several signaling pathways important for tumor growth. Other molecules, such as SGLT2 inhibitors, also show potential for slowing cell proliferation or attenuating inflammation. It should be noted, however, that these effects are not systematic. They actually depend on the type of cancer concerned or the specific molecule used.
This heterogeneity highlights the need to continue investigations. As Dr. Linong Ji, co-author of the analysis, suggests, if these medications remain essential for managing diabetes, their effects on a broader scale on cancer are not yet fully elucidated. The available data sometimes show contradictions and require consolidation through complementary work.
A fine understanding of these mechanisms could offer promising perspectives. In the long term, it could allow refining therapeutic strategies for patients facing both diabetes and cancer. It could also promote prevention approaches, particularly for populations at high risk for these two pathologies.
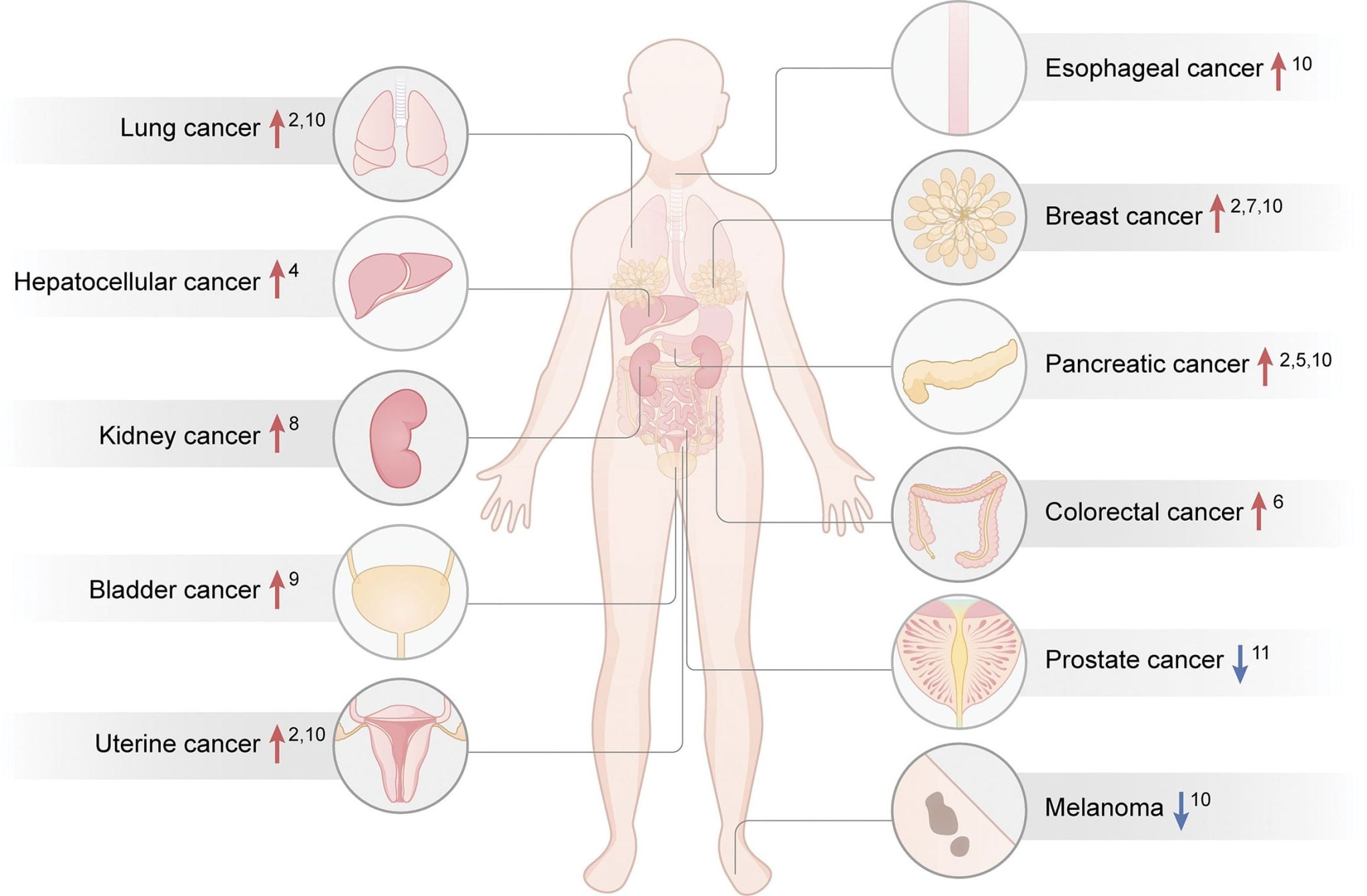
Infographic illustrating the link between type 2 diabetes and the increased (upward arrow) or reduced (downward arrow) risk for certain specific cancers.
Credit: Precision Clinical Medicine
Ongoing research thus paves the way for future clinical trials. Their objective will be to evaluate whether certain existing medications could be optimized or used in complement to conventional anticancer therapies.
How can a medication act on several diseases?
Medications are often designed to target a precise biological pathway linked to a disease. However, the organism functions as an interconnected network. A molecule that acts on a particular receptor or enzyme can therefore have repercussions on other processes, sometimes distant from its main effect. This is what is called pleiotropic effects.
These multiple effects can explain why a treatment for diabetes, such as metformin, could also influence cancer. By modifying cellular metabolism or the environment in which a tumor develops, the medication creates conditions less favorable to its growth. It does not directly attack cancer cells, but changes the terrain.
This approach opens possibilities for the reuse of existing medications. Instead of developing a new molecule from scratch, scientists explore whether a treatment already approved and well-known for one indication could be beneficial for another. This can accelerate research and offer new therapeutic options more quickly.
Nevertheless, this strategy requires rigorous validation. The effects observed in the laboratory or in certain studies must be confirmed by clinical trials specifically designed to evaluate efficacy and safety in the new context of the targeted disease.