Follow us on Google News (click on ☆)
In an article published in the journal Nature Communications, scientists reveal crucial information about the mechanism of Mavacamten, a therapeutic molecule recently approved by the FDA. This cutting-edge research paves the way for the development of precision medicine for heart diseases.
HCM is a public health issue affecting approximately one in 500 people. Clinically, these diseases are characterized by abnormal heart contractions that gradually lead to heart failure.
"These abnormal contractions are due to the presence of mutations expressed in the contractile muscle fibers called myosins, which act as the pump's motor. We know there are several hundred of these mutations today, with different molecular effects but similar symptoms." explains Dr. Julien Robert-Paganin.
Current treatments rely on invasive surgeries, up to heart transplantation in the disease's late stages, with significant consequences on patients' quality of life.
"A question arises from these data: is it possible to develop drugs capable of rectifying the heart's contraction force by directly modulating myosin activity?" continues Anne Houdusse.
Two molecules have these effects: Omecamtiv mecarbil, which activates myosin contraction, and Mavacamten, which inhibits it. To understand how these molecules mediate their opposite effects, scientists used X-ray crystallography to identify the binding site on myosin.
The study reveals that these two molecules, despite having opposite effects on myosin contraction, bind to the exact same spot on the muscle fiber. Detailed molecular dynamics studies show how these two drugs mediate their opposing effects. Although their target is the same, the molecules have different mobility and stability in the pocket, interacting differently with the myosin motor domain, explaining their inverse actions.
In addition to alleviating symptoms, these molecules can slow disease progression. The thickening of the heart wall, the root of long-term complications, is due to the abnormal contraction force of heart muscles. Studies have shown that by rectifying this force, the walls are less damaged, suggesting that taking such medication at early stages of the disease can reduce the risk of developing heart failure.
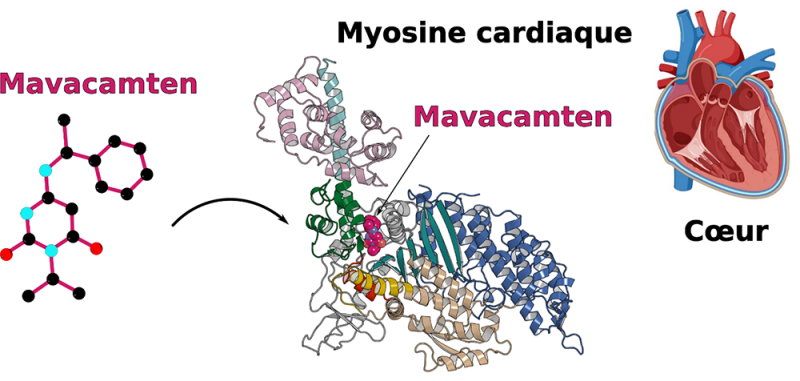
© Julien Robert-Paganin, Daniel Auguin and Anne Houdusse
For the continuation of this project, scientists are combining structural study with molecular dynamics analysis to characterize other therapeutic molecules.
"Our team is also comparing the mechanism of action of other therapeutic molecules. With the goal of developing precision medicine, we now need to test these drugs' efficacy for various heart diseases," indicates Julien Robert-Paganin.
They aim to better understand how muscle contraction is controlled to diversify molecules of interest capable of modulating the produced force.
"This study is a key step in our understanding of function modulators of molecular motors. While Mavacamten has just become available to patients, our research provides essential knowledge to inform doctors about its mechanism and better advise on future revolutionary treatments, which are now in phase 3 clinical trials for heart diseases," concludes Anne Houdusse.
Reference:
Omecamtiv mecarbil and Mavacamten target the same myosin pocket despite antagonistic effects in heart contraction
D. Auguin, J. Robert-Paganin, S. Réty, C. Kikuti, A. David, G. Theumer, A. W. Schmidt, H.-J. Knölker, A. Houdusse.
Nature Communications, June 7, 2024, https://doi.org/10.1038/s41467-024-47587-9