Major breakthrough in defeating cancer through radiotherapy 🧬
Published by Cédric,
Article author: Cédric DEPOND
Source: Nature Cell Biology
Other Languages: FR, DE, ES, PT
Article author: Cédric DEPOND
Source: Nature Cell Biology
Other Languages: FR, DE, ES, PT
Follow us on Google News (click on ☆)
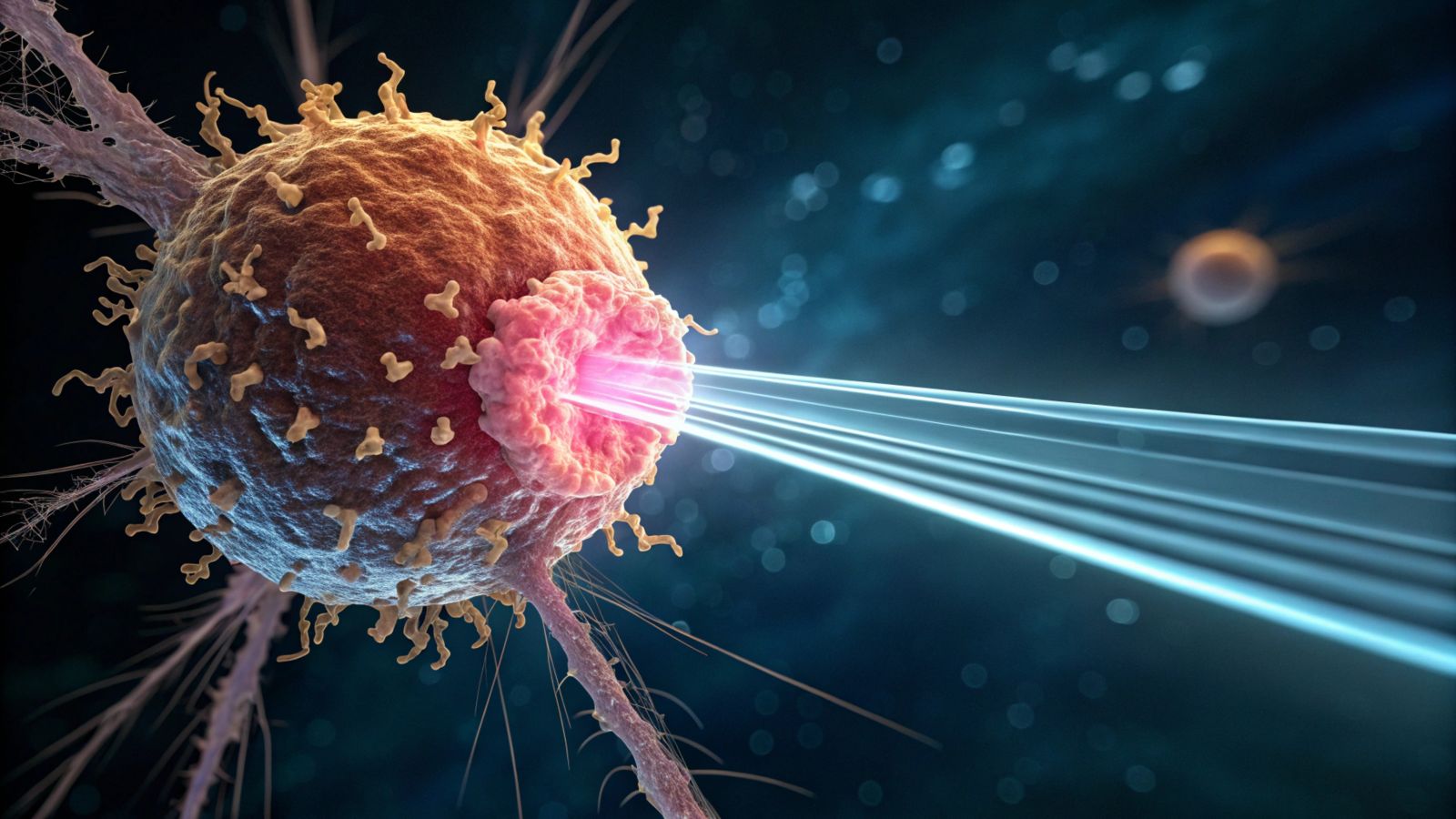
Radiotherapy is a cornerstone of cancer treatment, but its effectiveness varies depending on how tumor cells die. Some forms of cell death go unnoticed by the immune system, while others trigger a powerful immune response, enabling the body itself to fight the cancer. Understanding these differences is essential for improving existing therapies.
The role of DNA repair
The researchers discovered that DNA repair mechanisms play a central role in how cancer cells respond to radiotherapy. Normally, these mechanisms protect healthy cells, but in the case of massive damage, such as that caused by radiotherapy, they can influence the type of cell death.
When cancer cells repair their radiotherapy-damaged DNA using "homologous recombination," they die during cell division. This type of death goes unnoticed by the immune system, limiting the effectiveness of the treatment. Indeed, without an alert signal, the immune system cannot identify and attack the remaining cancer cells.
On the other hand, when other DNA repair mechanisms come into play, they produce byproducts resembling an infection. These byproducts activate the immune system, which then recognizes the cancer cells as a threat. This alert allows the immune system to destroy not only the damaged cancer cells but also any residual tumor cells, thereby reducing the risk of recurrence.
Blocking homologous recombination to activate immunity
By blocking homologous recombination, the researchers succeeded in altering how cancer cells die after radiotherapy. Thus, instead of dying silently during cell division, the cancer cells released byproducts that alerted the immune system, prompting it to destroy other cancer cells.
This discovery paves the way for combined treatments, associating radiotherapy and immunotherapy. By inhibiting homologous recombination, doctors could force cancer cells to die in a way that activates the immune system, thereby increasing the overall effectiveness of the treatment.
Technology at the heart of the discovery
The use of real-time microscopy allowed the researchers to track irradiated cells for a week. This technology revealed the complexity of cell death processes and was essential for understanding the mechanisms at play.
According to Professor Tony Cesare, this discovery is the result of six years of hard work. It offers new perspectives for improving cancer treatments, particularly by combining radiotherapy and immunotherapy to increase cure rates.
To go further: What is homologous recombination?
Homologous recombination is a DNA repair mechanism that allows cells to correct double-strand breaks, one of the most severe types of damage. This process uses a similar DNA sequence as a template to accurately repair the break, thereby preserving genome integrity.
Under normal conditions, homologous recombination is essential for maintaining genetic stability and preventing mutations that could lead to cancer. However, in the context of cancer treatment, this mechanism can also protect tumor cells by repairing the damage caused by radiotherapy.
Cancer cells that heavily rely on homologous recombination, such as those carrying BRCA2 mutations, are particularly vulnerable when this mechanism is blocked. This explains why homologous recombination inhibitors are promising for enhancing the effectiveness of cancer treatments.
What is radiotherapy?
Radiotherapy is a medical treatment that uses high-energy radiation to destroy cancer cells or prevent their growth. It works by damaging the DNA of tumor cells, preventing them from multiplying and leading to their death.
This treatment is widely used for many types of cancer, either alone or in combination with other therapies such as surgery or chemotherapy. Radiotherapy can be administered externally, via a machine that directs the rays toward the tumor, or internally, by placing a radioactive source near the cancer cells.
Although it primarily targets cancer cells, radiotherapy can also affect nearby healthy cells, which explains some side effects. However, modern techniques allow for minimizing this damage by precisely targeting the tumor.