Follow us on Google News (click on ☆)
A study supported by ANRS MIE and conducted by teams at Inserm, the University of Bordeaux, and the CNRS (ImmunoConcEpT), examined the evolution of CD8+ T lymphocytes after several decades of antiretroviral treatment in individuals living with HIV.
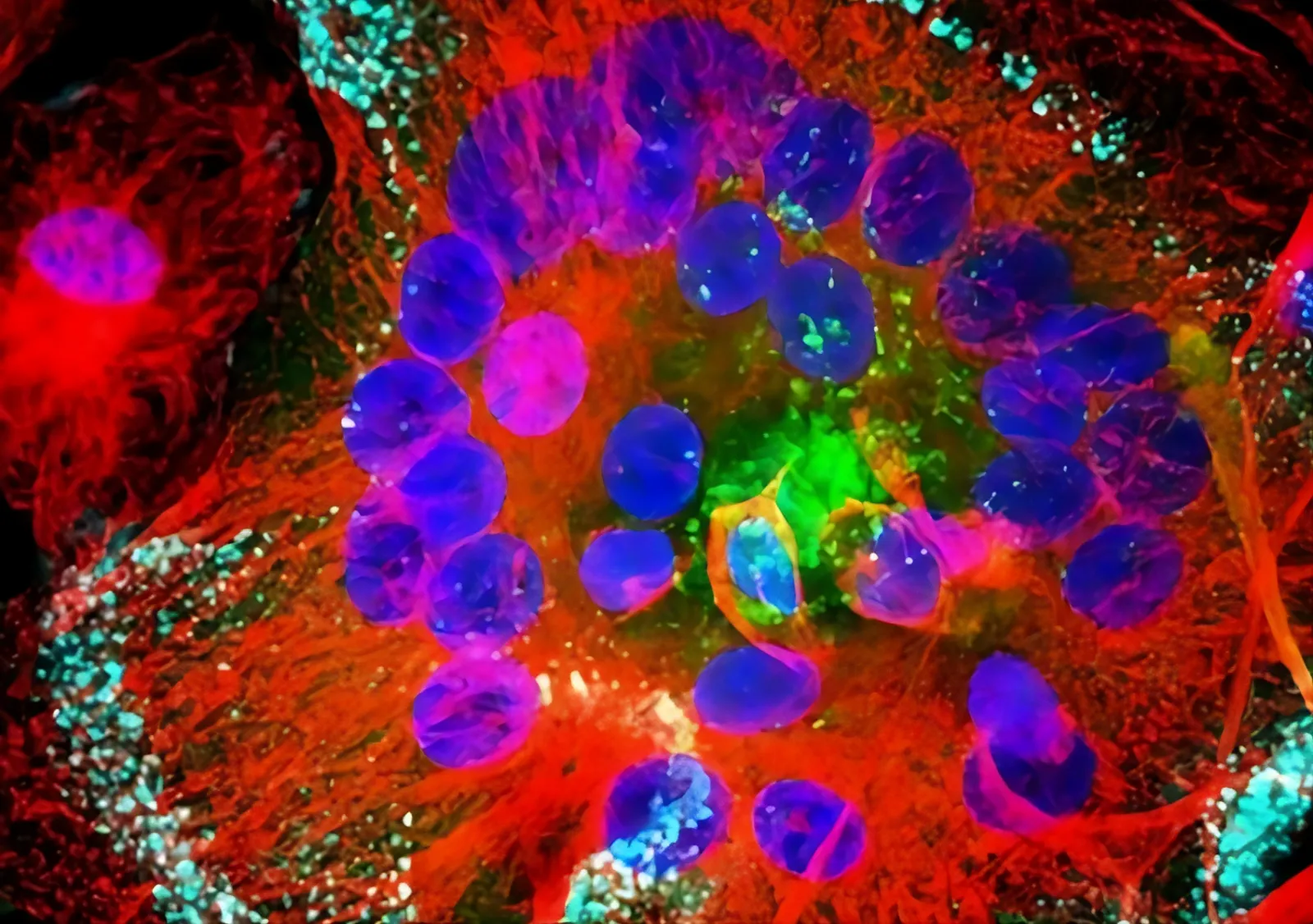
Macrophages infected by HIV: Viral proteins are shown in green, microtubules in red, and nuclei in blue. Nuclei size: 5µm (microns)
© Inserm/Institut Curie, R. Gaudin/P. Bernaroch
Contrary to scientific expectations, the results showed a renewal of CD8+ T cells, suggesting the immune system's ability to generate new responses. The results of this research were recently published in the journal Nature Immunology.
CD8+ T lymphocytes are essential for the effective immune control of viruses or cancers.
However, in the case of HIV, the fate of these cells decades after the initial immune response to the virus was induced remains poorly understood. Victor Appay's team, led by the Inserm research director,[1] questioned the status of CD8+ lymphocytes after years of infection controlled by antiretroviral treatments.
This study was based on a unique cohort of individuals living with HIV-1, all of whom had donated historical samples dating back to the early epidemic in the 1990s (IMMUNOCO cohort, established at the Salpêtrière Hospital, AP-HP and funded by ANRS MIE).
The average clinical follow-up of the patients was 27 years, an unusually long timeframe. Furthermore, the aging of the patients, whose average age increased over the long-term follow-up, represents an additional factor to consider, given the weakening of immune defenses with age. Out of 152 patients in the cohort, 28 were located for this new study, and samples were collected from 20 of them.
Surprisingly, and contrary to expectations, the results showed that in 11 patients where HIV-specific CD8+ T cells were detected, these cells exhibited characteristics of rejuvenation.
This phenomenon is due to the emergence of new, younger, and more functional cells within the HIV-specific CD8+ T cell compartment. These new cells outcompete older ones in the context of immune reconstitution achieved through long-term antiretroviral treatment. This is described as a "clonal succession process" within the populations of HIV-1-specific CD8+ T lymphocytes, leading to their rejuvenation. It demonstrates the immune system's resilience and ability to generate new responses.
These findings represent a significant contribution to our understanding of virus-specific T cell immunity, 40 years after the initial discovery of HIV-1. The next step is to investigate in vitro, and later in preclinical and clinical models, how to stimulate these new CD8+ T cells with renewed functional potential to generate effective responses.
The implications of this research extend beyond HIV-1. The discovery that the exhaustion and senescence of T cells can be naturally overcome to generate functional immunity highlights the immune system's resilience even after decades, in extreme circumstances.
This research project could transform current therapeutic approaches not only against HIV but also other diseases such as SARS-CoV-2 and cancer, particularly among aging populations.
"These results offer new hope for the development of HIV-1 cure strategies based on the reinvigoration of functional CD8+ T cell responses after long-term treatment." says Victor Appay, University of Bordeaux.
Note:
[1] Victor Appay is co-leader of the "Vulnerability and Aging of the Immune System" team, Inserm U1303, within the ImmunoConcept unit.